Featured new articles related to intranasal drug delivery:
January-March 2013
Based on another request, we have posted a set of Pre-hospital teaching slides that have audio embedded. You can download these, eliminate any slides you wish and customize them to fit your needs.
EMS teaching slide sets with audio embedded
Intranasal drug delivery - General principles (20 minutes)
Intranasal drug delivery - Clinical application (30 minutes)
___________________________________
Etteri, M. and A. Bellone,
Intranasal Fentanyl for analgesia in adults with acute renal colic.
Emergency Care Journal, 2012. 8(2): p. 13-18.
Objectives: The usual treatment of pain in acute renal colic is analgesic
in intravenous (IV) route. We tried a rapid, non painful, non-invasive
route of administration using intranasal fentanyl versus IV standard
treatment (non steroidal anti-inflammatory drug (NSAIDs) plus morphine)
for the relief of pain in renal colic presenting to an Emergency
Department (ED). Methods: We conducted a prospective non-blinded
randomized clinical trial. A sample of 63 adult patients with clinical
diagnosis of acute renal colic was included to receive either
intravenous morphine (5 mg) plus ketorolac (30 mg) or intranasal
fentanyl (3 µg/kg). Pain score were rated by using a 10 cm visual
analogue scale at 0,30 and 60 minutes after the treatment. Primary
outcome was pain reduction. Secondary outcomes were adverse events and
rescue treatment. Results: Sixty-three patients were enrolled. Thirty
patients received nasal fentanyl and thirty-three received intravenous
morphine plus ketorolac. Morphine-ketorolac therapy was statistically
significant more effective than nasal fentanyl therapy in visual analog
scores at 30 minutes: the difference in mean visual analog scale between
the two groups was 1.74 cm (95% confidence interval 0.29 to 3.2;
P=0.018) at 30 minutes. There were not statistically significant
differences between the two groups at 60 minutes. There were no
significant differences between the groups with regard to secondary
outcomes (adverse events and rescue treatment). Conclusions: A
combination of intravenous morphine plus ketorolac offers pain relief
superior to nasal fentanyl treatment for ED patients with acute renal
colic
Click here for the journals link to the article (free)
Web site Editorial comments:
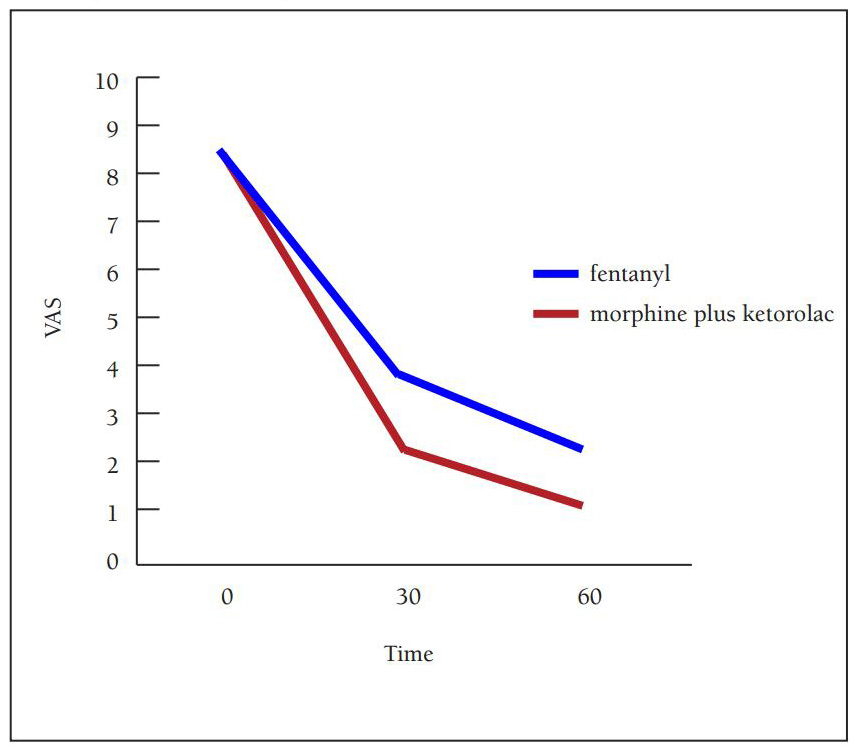
This is a very nice clinical trial that compared IV
morphine plus IV ketorolac (5 mg / 30 mg) to intranasal fentanyl (3
mcg/kg of 50 mcg/ml solution) for the treatment of acute renal colic in
adults. Not surprisingly, the IV formulation was superior in efficacy.
However, it is still quite impressive how the nasal group faired in
terms of pain control for such an uncomfortable condition (see the
graph). Pain scores on a 10 cm VAS at entry, 30 minute and 60 minutes
for the morphine/ketorolac IV arm were 8.6 / 2.3 / 1.1 respectively. For
the intranasal fentanyl arm they were 8.8 /4.0 / 2.2 respectively. The
authors conclude that for a condition as painful as renal colic, IV
morphine and ketorolac is the first choice of therapy, while nasal
fentanyl might be appropriate in a less controlled setting such as out
of hospital or nurse initiated setting.
It is not surprising that the IV combination of an opiate plus
a NSAID worked better than an opiate alone for 2 reasons. First generic
concentrations of fentanyl tend to be a little less effective in adults
due to volume issues and second because non-steroidal anti-inflammatories
are a mainstay for successful therapy of renal colic. They are in
reality the best treatment over time, but take longer to work so we tend
to add an opiate to get pain more rapidly in control. I wonder if a
combination of concentrated fentanyl or generic sufentanil PLUS an oral
or nasal NSAID might not have changed these results. I have no research
data to support this opinion but do have personal experience (nasal
sufentanil plus oral ibuprofen) suggesting it is very effective. Future
investigators should strongly consider these minor protocol changes –
the authors actually admit the lack of a NSAID is a limitation to their
study design. I do agree
with the investigators that IV therapy is preferred if possible because
these patients frequently need multiple doses of drugs and nausea
medications and repeat evaluations, need their blood drawn to evaluate
renal function (so get a needle stick anyhow), etc. Never the less this
is a great study and helps us define the niche (or lack of niche) for
nasal drugs in our daily practice.
Pubmed link: not on Pubmed - go here instead - http://www.pagepressjournals.org/index.php/ecj/article/view/1072
___________________________________
Coffin, P.O. and S.D. Sullivan,
Cost-effectiveness of distributing naloxone to heroin users for lay
overdose reversal. Ann Intern Med, 2013. 158(1): p. 1-9.
Compton, W.M., et al.,
Expanded access to opioid overdose intervention: research, practice, and
policy needs. Ann Intern Med, 2013. 158(1): p. 65-6.
BACKGROUND: Opioid overdose is a leading cause of accidental death in the
United States. OBJECTIVE: To estimate the cost-effectiveness of
distributing naloxone, an opioid antagonist, to heroin users for use at
witnessed overdoses. DESIGN: Integrated Markov and decision analytic
model using deterministic and probabilistic analyses and incorporating
recurrent overdoses and a secondary analysis assuming heroin users are a
net cost to society. DATA SOURCES: Published literature calibrated to
epidemiologic data. TARGET POPULATION: Hypothetical 21-year-old novice
U.S. heroin user and more experienced users with scenario analyses. TIME
HORIZON: Lifetime. PERSPECTIVE: Societal. INTERVENTION: Naloxone
distribution for lay administration. OUTCOME MEASURES: Overdose deaths
prevented and incremental cost-effectiveness ratio (ICER). RESULTS OF
BASE-CASE ANALYSIS: In the probabilistic analysis, 6% of overdose deaths
were prevented with naloxone distribution; 1 death was prevented for
every 227 naloxone kits distributed (95% CI, 71 to 716). Naloxone
distribution increased costs by $53 (CI, $3 to $156) and
quality-adjusted life-years by 0.119 (CI, 0.017 to 0.378) for an ICER of
$438 (CI, $48 to $1706). RESULTS OF SENSITIVITY ANALYSIS: Naloxone
distribution was cost-effective in all deterministic and probabilistic
sensitivity and scenario analyses, and it was cost-saving if it resulted
in fewer overdoses or emergency medical service activations. In a
"worst-case scenario" where overdose was rarely witnessed and naloxone
was rarely used, minimally effective, and expensive, the ICER was $14
000. If national drug-related expenditures were applied to heroin users,
the ICER was $2429. LIMITATION: Limited sources of controlled data
resulted in wide CIs. CONCLUSION: Naloxone distribution to heroin users
is likely to reduce overdose deaths and is cost-effective, even under
markedly conservative assumptions. PRIMARY FUNDING SOURCE: National
Institute of Allergy and Infectious Diseases.
In an accompanying editorial, Compton et al review the FDA views on
the topic – which are extremely favorable towards prescription home
naloxone and eventually over the counter naloxone. At this point the FDA
is fully aware of the off-label lay person use of naloxone both nasally
and Intramuscularly and applauds this movement but hopes to encourage
the pharmaceutical industry to develop easily administered and more
highly controlled forms of this medication.
Web site Editorial comments:
Is a year of
life worth $438-$14,000 to you? Is it worth saving a human life – often
a young adult - so they can
go on to experience life for decades to come? I doubt this is a very
hard decision and I find it amazing and sad when I hear some clinicians
or politicians comment on the ethics of distributing naloxone to lay
people. Have they forgotten
why we have entered the practice of medicine, have they really lost
their human compassion for the value of someone else’s life? Do they
truly believe they can judge a life worth saving (for a few hundred
dollars per year no less) versus one that is not?
Pubmed link: http://www.ncbi.nlm.nih.gov/pubmed/23277895
___________________________________
Yeaman F, Oakley E, Meek R, Graudins A. Sub-dissociative dose intranasal
ketamine for limb injury pain in children in the emergency department: A
pilot study. Emerg Med Australas 2013;25:161-7.
OBJECTIVE: The present study aims to conduct a pilot study examining the
effectiveness of intranasal (IN) ketamine as an analgesic for children
in the ED. METHODS: The present study used an observational study on a
convenience sample of paediatric ED patients aged 3-13 years, with
moderate to severe (>/=6/10) pain from isolated limb injury. IN ketamine
was administered at enrolment, with a supplementary dose after 15 min,
if required. Primary outcome was change in median pain rating at 30 min.
Secondary outcomes included change in median pain rating at 60 min,
patient/parent satisfaction, need for additional analgesia and adverse
events being reported. RESULTS: For the 28 children included in the
primary analysis, median age was 9 years (interquartile range [IQR]
6-10). Twenty-three (82.1%) were male. Eighteen (64%) received only one
dose of IN ketamine (mean dose 0.84 mg/kg), whereas 10 (36%) required a
second dose at 15 min (mean for second dose 0.54 mg/kg). The total mean
dose for all patients was 1.0 mg/kg (95% CI: 0.92-1.14). The median pain
rating decreased from 74.5 mm (IQR 60-85) to 30 mm (IQR 12-51.5) at 30
min (P < 0.001, Mann-Whitney). For the 24 children who contributed data
at 60 min, the median pain rating was 25 mm (IQR 4-44). Twenty (83%)
subjects were satisfied with their analgesia. Eight (33%) were given
additional opioid analgesia and the 28 reported adverse events were all
transient and mild. CONCLUSIONS: In this population, an average dose of
1.0 mg/kg IN ketamine provided adequate analgesia by 30 min for most
patients.
Web site Editorial comments:
Editorial
comment: Here is the first study that many readers have been awaiting
describing the efficacy of intranasal ketamine for treatment of acute
pain. It is a small, preliminary trial but the results are promising and
it gives us a starting dose – 1 mg/kg of intranasal ketamine. This drug
might be used to complement fentanyl if the initial dose of fentanyl is
effective, or visa versa – given first line and followed with Fentanyl
if additional pain medication is required. The study also points out a
concept that some clinicians still are not familiar with – the concept
of titration of pain medication via the NASAL route just as we all do
via the intravenous route. Within 30 minutes, using no IV access, these
children had their pain scores down by 44 mm. This is almost identical
to that seen with titrated fentanyl in the Borland study from 2007. Here
is another tool in our armamentarium for treating acute pain –
painlessly.
Pubmed link: http://www.ncbi.nlm.nih.gov/pubmed/?term=yeaman+and+intranasal+ketamine
___________________________________
Title:
Abstract
Web site Editorial comments:
Pubmed link:
 Therapeutic
Intranasal Drug Delivery
Therapeutic
Intranasal Drug Delivery